Research transforms care for people with multiple sclerosis
Our researchers are leading the way to more effective, affordable, and equitable care.
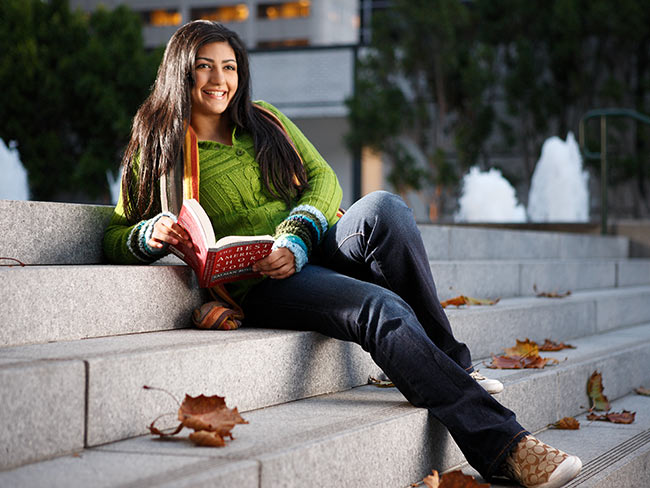
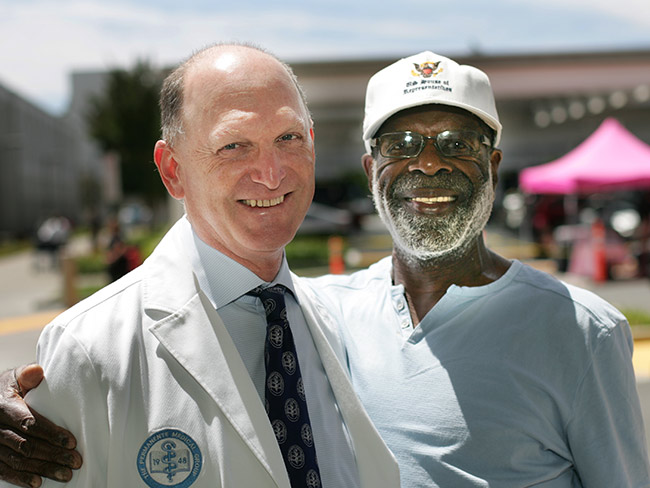
Annette Langer-Gould, MD, PhD, studies treatments to improve care for people with MS. Jacques Roussel is a patient partner in one of her studies.
Treatment for multiple sclerosis needs to change. At Kaiser Permanente, it already has.
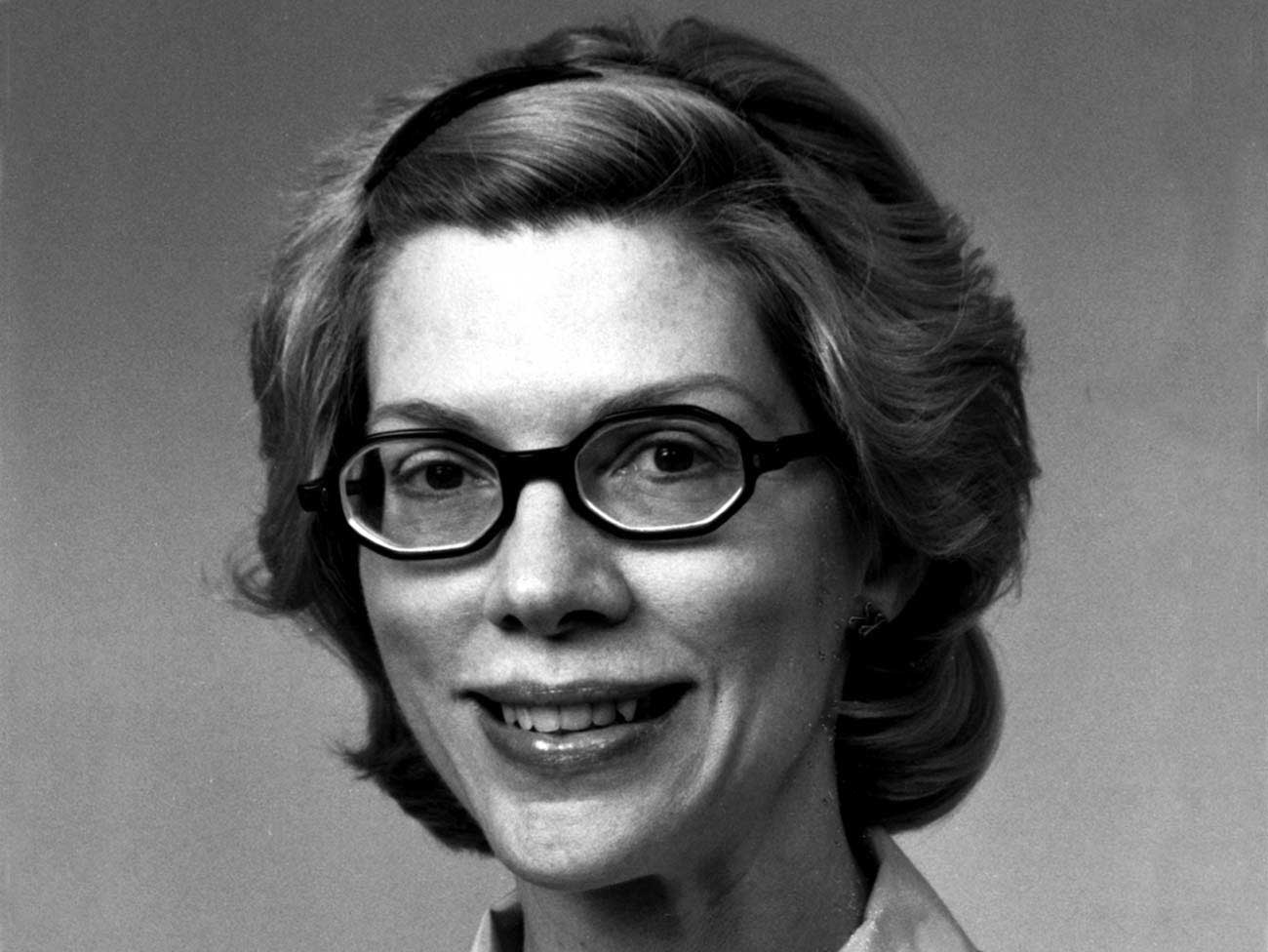
We’ve improved care thanks to research conducted by Annette Langer-Gould, MD, PhD, and her colleagues.
Dr. Langer-Gould wants the rest of the world to follow. She co-authored an article in the journal Neurology urging the medical community to adopt use of a medication that has the potential to improve care for many patients.
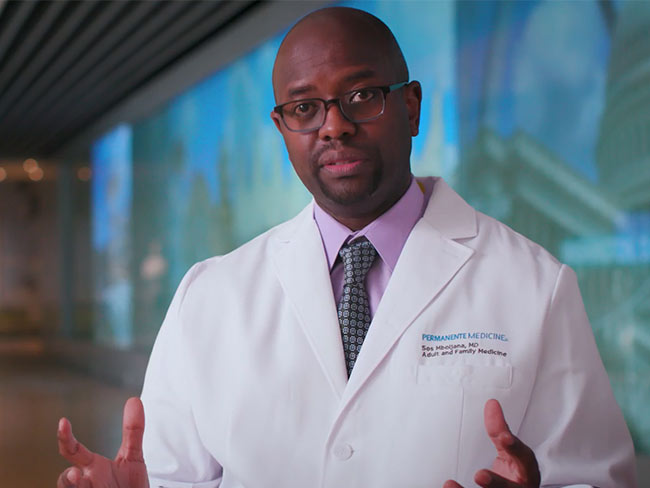
Dr. Langer-Gould, a neurologist and a scientist who studies MS, discusses what she’s learned through her research.
What is MS?
MS is a disease that affects the brain and spinal cord, often leading to permanent disability. It cannot be cured. But medications can help reduce the risk of disability.
Nearly a million people in the United States have MS. For most people, the disease starts with a rather sudden onset of symptoms. Those symptoms may go away or lessen with time. If new symptoms appear or old symptoms return for a period of time, it’s called a relapse.
Why does MS treatment need to change?
People with more aggressive MS benefit from stronger drugs. However, in the United States, many people can’t afford the copays. Sometimes people don’t get the treatment they need and become disabled.
At Kaiser Permanente in Southern California, our Multiple Sclerosis Treatment Optimization Program ensures that more people with relapsing MS receive highly effective drugs as early in the disease course as possible.
Key to the program is our increased use of a drug called rituximab. This drug is more traditionally used for cancer and other diseases. But evidence shows it’s safe and highly effective for relapsing MS. And it costs much less than other options.
Many insurance carriers in the United States and Europe limit coverage of rituximab for treating MS. They’ve cited a lack of regulatory approval for use of the drug to treat MS. But that may be changing.
The World Health Organization now lists rituximab as an essential drug for MS. I hope other organizations will follow. Wider use could have significant benefits for patients and could reduce inequities.
How has your research led you to push for a shift?
A study we published in 2022 found that MS relapse rates plummeted for Kaiser Permanente members in Southern California during the initial rollout of our program. Thanks in part to the lower cost of rituximab, the cost of treatment has fallen.
And patients say they love rituximab. Besides being effective and affordable, it’s long-lasting, so they don’t need to come to the office as often. That means more people tend to stick with treatment over time.
What’s more, research in Sweden showed similar benefits of rituximab for patients. The country’s health care system has now approved it for MS. It really seems to be a game changer.
What drew you to study MS?
I began seeing MS patients as a medical resident and PhD student. It’s a chronic disease, so it gave me an opportunity to build rewarding, long-term relationships with patients. I also realized studying MS would be a chance to fight for underserved patients.
Our success with MS highlights Kaiser Permanente’s use of evidence-based medicine. We’re improving care based on evidence gathered through our research. And we hope the rest of the country follows our lead.
-
Social Share
- Share Research Transforms Care for People With Multiple Sclerosis on Pinterest
- Share Research Transforms Care for People With Multiple Sclerosis on Linkedin
- Share Research Transforms Care for People With Multiple Sclerosis on Twitter
- Share Research Transforms Care for People With Multiple Sclerosis on Facebook
- Print Research Transforms Care for People With Multiple Sclerosis
- Email Research Transforms Care for People With Multiple Sclerosis

April 23, 2024
We’re rising up to help prevent falls
Kaiser Permanente is committed to finding ways to help reduce falls in …

April 17, 2024
5 common health conditions men don’t like to talk about
Some of the most common conditions affecting men carry a social stigma …

April 9, 2024
Denver Fire Department annual blood work screenings triple
It’s easy to put off recommended health screenings, and sometimes even …

April 1, 2024
Lynch syndrome: Managing the risk of hereditary colon cancer
Lynch syndrome is a gene mutation that increases colon cancer risk. Learn …

March 19, 2024
Fostering responsible AI in health care
With the right policies and partnerships, artificial intelligence can lead …

March 14, 2024
Healthy kidneys support overall good health
Kaiser Permanente excels in preventing, detecting, and treating kidney …

March 13, 2024
A call to 'Connect' to uncover the causes of cancer
Learn more about a study to help prevent cancer.

March 12, 2024
In-home recovery restores harmony to life
Colorado musician back with the band thanks to new virtual cardiac rehab …

March 6, 2024
Are you dreading the spring season?
A new Kaiser Permanente facility in Bellflower, California, makes customized …

February 21, 2024
From planning his funeral to celebrating his wedding
Gabriel Abarca had no hope for his future. Then the team at Kaiser Permanente …

February 8, 2024
Road to heart health: Living well
You have only one heart. ‘Prescribe’ yourself a few changes to help protect …

February 1, 2024
Road to heart health: Know your risk factors
One of the best ways to prevent future heart conditions is knowing what …

January 31, 2024
Prioritizing policies for health and well-being in Colorado
CityHealth’s 2023 Annual Policy Assessment awards cities for their policies …

December 12, 2023
Hundreds attend first Food Is Medicine Summit
Attendees look at ways to get healthy food to people who don’t have enough …

December 6, 2023
Leading research with gratitude
Learn how you can participate in a study to uncover what causes cancer …

December 6, 2023
Leaders named among health care’s most influential
Greg A. Adams; Maria Ansari, MD, FACC; and Ramin Davidoff, MD, have been …

October 23, 2023
The future of health care is digital
Nari Gopala, Kaiser Permanente’s chief digital officer, answers 3 questions …

October 4, 2023
An easier way to manage multiple prescriptions
If you have an ongoing health condition, you know it can be tricky to keep …

September 27, 2023
10 school districts receive next round of RISE grants
The Thriving Schools program helps educators and students in Colorado integrat …

September 19, 2023
Is telehealth right for you?
Members give video visits high marks — and with a few simple tips, you …

September 13, 2023
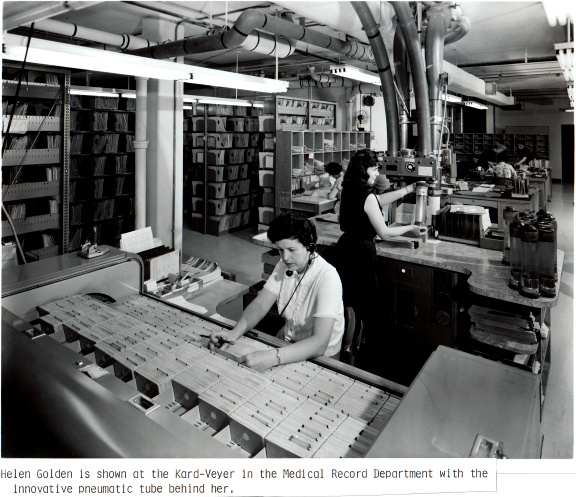
Transforming the medical record
Kaiser Permanente’s adoption of disruptive technology in the 1970s sparked …

August 16, 2023
Cervical cancer screening: Exploring the at-home HPV test
Kaiser Permanente is at the forefront of cervical cancer research. Find …

August 15, 2023
As temperatures rise, so does the risk of heart problems
A Kaiser Permanente cardiologist shares advice on how to stay safe, what …

August 15, 2023
Screening for breast cancer: Mammogram guidelines
Mammograms can help detect breast cancer early, when it’s easier to treat. …
August 14, 2023
Tips for ensuring a safe and healthy college experience
Students should study up on their care options to ace their school experience. …

August 14, 2023
Marla’s story: Surviving acute promyelocytic leukemia
After a diagnosis for a rare type of blood cancer, Marla Marriott got high-qua …
August 4, 2023
Eating well and adopting healthy habits helps prevent cancer
Learn how lifestyle medicine is part of cancer care at Kaiser Permanente.

June 15, 2023
Stay safe while having fun in the sun
Tips for preventing sunburn and decreasing the risk of skin cancer.

June 14, 2023
5 easy ways to reduce heart disease risk
A reminder that men and women can assert control over risk factors that …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

April 25, 2023
Nari Gopala named chief digital officer
Gopala will be responsible for leading Kaiser Permanente's digital transformat …

April 14, 2023
The importance of screening for gestational diabetes
Gestational diabetes poses a significant risk to women of color, particularly …

April 7, 2023
Increasing access to health care
Kaiser Permanente launches new mobile health vehicle on Oahu.

March 14, 2023
Colorectal cancer on the rise among younger adults
Learn why early screening is crucial for prevention and treatment.

March 6, 2023
Living with long COVID
From avid snowboarder to chronically ill patient. How Kaiser Permanente …

March 6, 2023
Have shots, will travel
Hawaii community vaccination team’s pop-up events with COVID-19 and flu shots.

March 1, 2023
Spring forward: How to prepare for losing an hour of sleep
A sleep expert shares 4 practical tips for coping with the time shift and …

February 27, 2023
Teaching flu a lesson
School-based flu vaccination clinics made it safe and convenient for students …

January 27, 2023
Timely flu vaccinations at community events
Proactive flu prevention outreach in Downey, California.

December 22, 2022
Denver earns an overall gold medal
CityHealth recognizes Denver for its leadership in supporting policies …

December 6, 2022
Building stronger, healthier communities at community event
Volunteers offered preventive care, first aid, cooling stations, and complimen …

November 16, 2022
Passport to preventive care
Special event helps Latino community ensure their flu vaccinations and …
November 11, 2022
Our integrated care model
We’re different than other health plans, and that’s how we think health …

October 6, 2022
We’re a Fast Company Innovation by Design winner
Kaiser Permanente is the first health care organization to win Design Company …

October 3, 2022
Flu shots save lives and offer proven protection
Black people, Latinos, and people over 65 years of age are especially vulnerab …
October 1, 2022
Innovation and research
Learn about our rich legacy of scientific research that spurred revolutionary …

August 17, 2022
2021 annual report sheds light on another challenging year
We reflect on 3 major COVID-19 surges, urgent vaccination efforts, and …

August 16, 2022
Seconds count: Know the signs of a stroke
A Kaiser Permanente physician shares why quick detection and expert treatment …

July 29, 2022
Helping community members access nutritious meals
Los Angelenos in need enjoy access to quality food, thanks to partnerships …

June 14, 2022
Treatment for addiction to prescription pain pills
He needed help coping with back pain while ending his reliance on opioids. …

June 7, 2022
The secret to a long life: Keep up with health screenings
For men who often resist regular doctor visits and health screenings, making …

June 6, 2022
New approach reduces colon cancer deaths
Kaiser Permanente reduces colon cancer deaths in its Southern California …

June 6, 2022
Get the better of your anger
Stress can easily become anger. But you can practice self-care to head …

May 5, 2022
Research study will inform the future of cancer prevention
Connect for Cancer Prevention Study’s goal to recruit 200,000 participants …

April 22, 2022
Targeting testicular cancer by pooling knowledge
Urologists and oncologists work with research and technology partners to …

November 12, 2021
Dental visit speeds cancer diagnosis and treatment
A reminder to complete a routine mammogram — and early detection — helped …

September 10, 2021
‘Baby in the drawer’ helped turn the tide for breastfeeding
This innovation in rooming-in allowed newborns to stay close to mothers …

September 9, 2021
How to lower your risk of dementia
It’s never too late (or too soon) to take preventive steps. And, with a …
August 13, 2021
Remote patient monitoring improves care for chronic disease
If you have a chronic condition such as high blood pressure or diabetes, …

July 30, 2021
Pairing doctors with your devices for improved health
Wellness and fitness-tracking devices can help doctors and patients coordinate …

July 2, 2021
Fireworks can cause wildfires, serious injury, and death
This Fourth of July, celebrate safely with family and friends.

May 24, 2021
Supporting access to telehealth for vulnerable populations
Kaiser Permanente grants help fund community organizations working to expand …

February 22, 2021
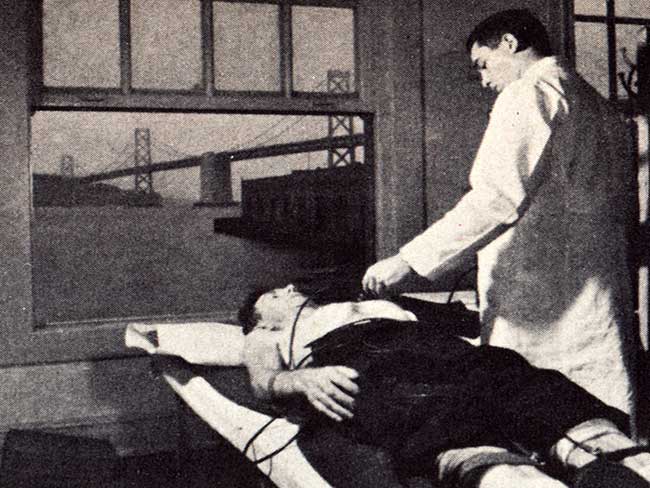
The Permanente Richmond Field Hospital
Forlorn and all but forgotten, it played a proud role during the World …

February 4, 2021
A passion for the practice of cardiology
Dr. Chileshe Price shares her commitment to advancing cardiac care through …

January 15, 2021
The fastest path to care
Available 24/7 with no appointment, e-visits offer Kaiser Permanente members …

September 28, 2020
A legacy of disruptive innovation
Proceeds from a new book detailing the history of the Kaiser Foundation …
August 26, 2020
Kaiser Permanente’s pioneering nurse-midwives
The 1970s nurse-midwife movement transformed delivery practices.

July 21, 2020
Diagnostic and preventive care is in our DNA
A routine screening helped detect Bill Walsh’s cancer before it became …

July 1, 2020
A breakout moment for virtual care
Kaiser Permanente’s fully integrated telehealth capabilities place quality …

June 4, 2020
A role model for quality, innovation, and transformation
Nation’s health care leaders and clinicians in annual survey point to Kaiser …

February 20, 2020
Bringing healing home with virtual cardiac rehabilitation
Michelle Wofford gets a new lease on life after a serious cardiac event.

August 2, 2019
Thriving with 1960s-launched KFOG radio
Kaiser Broadcasting radio connected listeners, while TV stations brought …

February 5, 2019
Mobile clinics: 'Health on wheels'
Kaiser Permanente mobile health vehicles brought care to people, closing …

April 30, 2018
Nursing pioneers leads to a legacy of leadership
Kaiser Foundation School of Nursing students learned a new philosophy emphasiz …

April 19, 2018
Wasting nothing: Recycling then and now
Environmentalism was a common practice at the Kaiser shipyards long before …

April 12, 2018
Harold Hatch, health insurance visionary
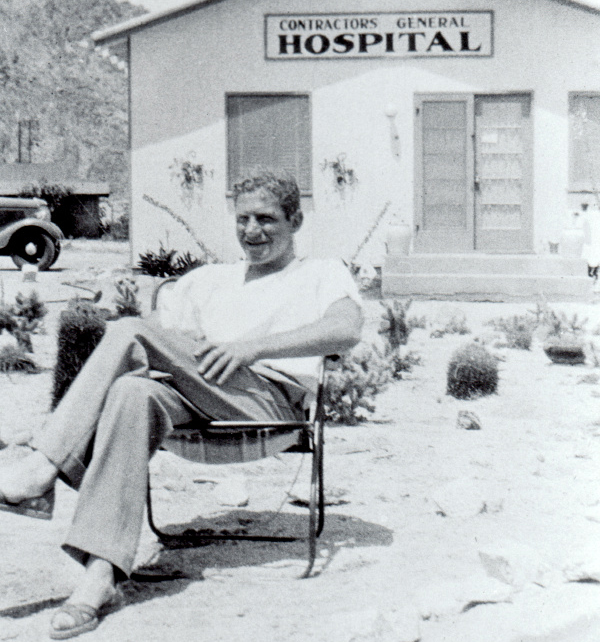
The founding of Kaiser Permanente's concept of prepaid health care in the …
March 26, 2018
5 physicians who made a difference
Meet 5 outstanding doctors who advanced the practice of medical care with …
December 19, 2017
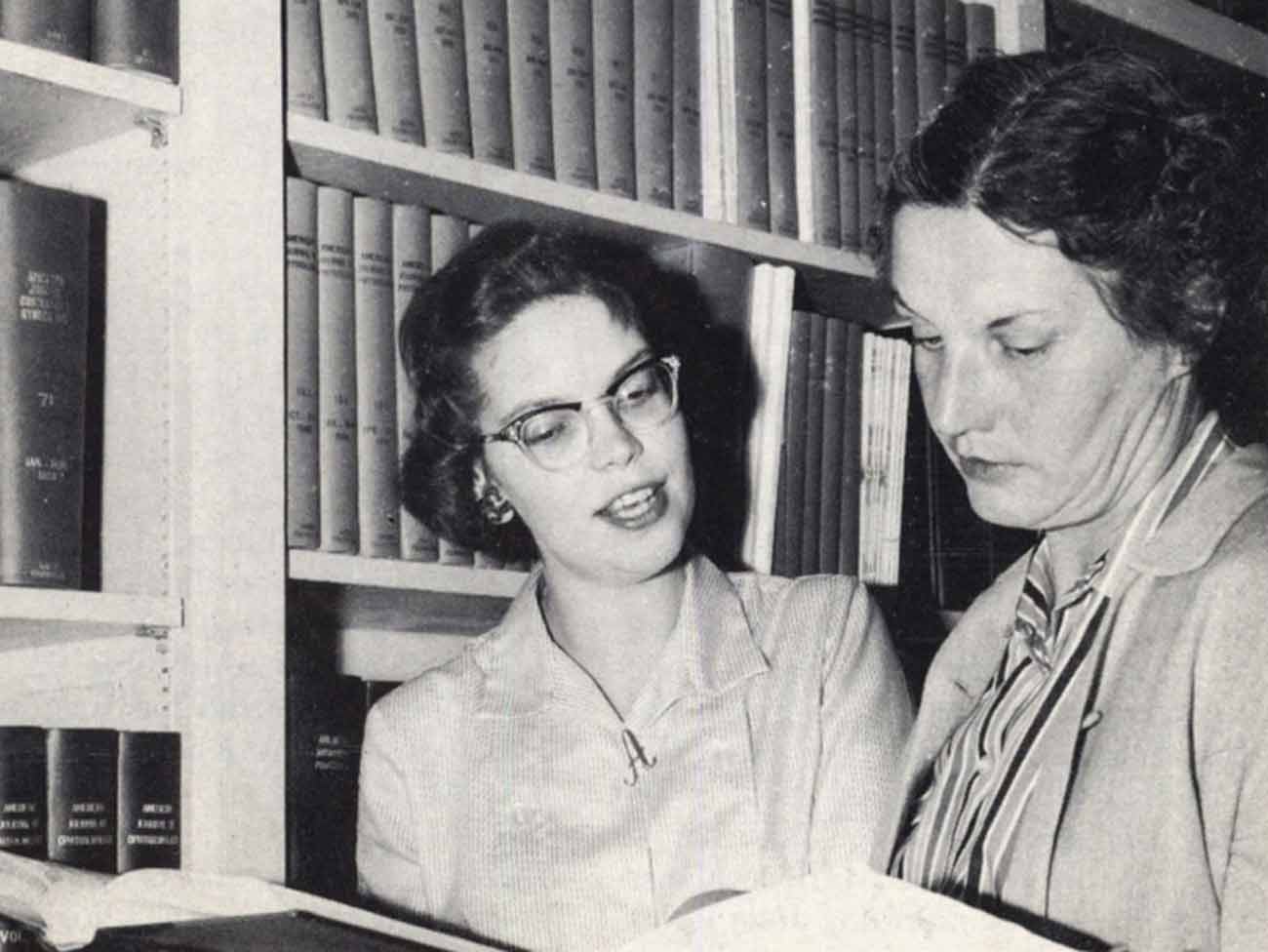
From boats to books: A history of Kaiser Permanente’s medical libraries
Kaiser Permanente librarians are vital in helping clinicians remain updated …

October 12, 2017
An experiment named Fabiola
Health care takes root in Oakland, California.

August 15, 2017
Sidney R. Garfield, MD, on medical care as a right
Hear Kaiser Permanente’s physician co-founder talk about what he learned …

August 10, 2017
‘Good medicine brought within reach of all'
Paul de Kruif, microbiologist and writer, provides early accounts of Kaiser …

July 14, 2017
Kaiser’s role in building an accessible transit system
Harold Willson, an employee, and an advocate for accessible transportation, …

July 7, 2017
Mending bodies and minds — Kabat-Kaiser Vallejo
The expanded new location provided care to a greater population of members …
June 23, 2017
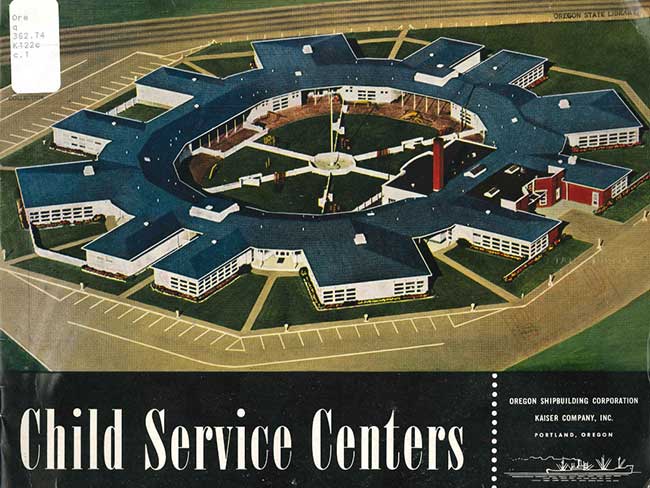
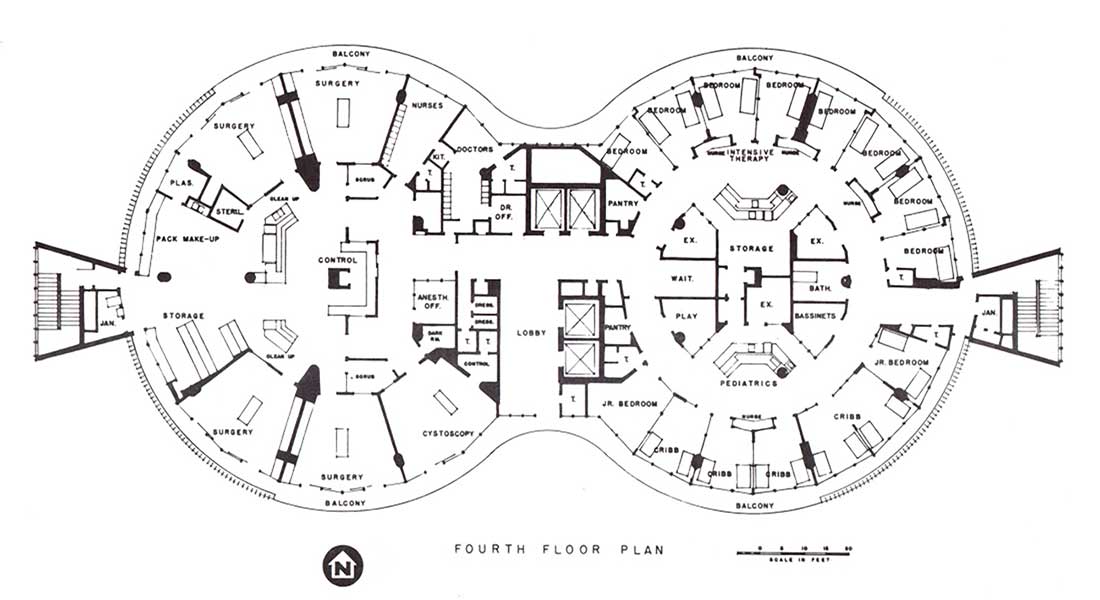
No getting round it: An innovative approach to building design
Kaiser Permanente incorporated innovative circular architectural designs …

June 14, 2017
Kabat-Kaiser: Improving quality of life through rehabilitation
When polio epidemics erupted, pioneering treatments by Dr. Herman Kabat …

June 9, 2017
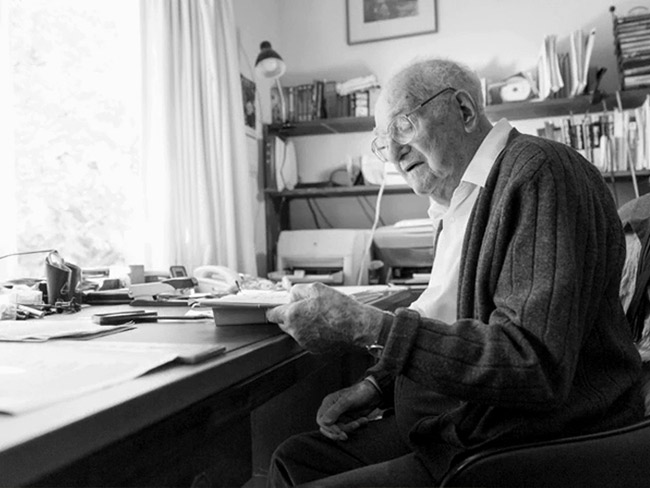
Edmund (Ted) Van Brunt, pioneer of electronic health records, dies at age …
Throughout his career, Dr. Van Brunt applied computers and databases in …

May 4, 2017
How a Kaiser Permanente nurse transformed health education
Kaiser Permanente's Health Education Research Center and Health Education …
March 1, 2017
Screening for better health: Medical care as a right
When industrial workers joined the health plan, an integrated battery of …
February 17, 2017
Experiments in radial hospital design
The 1960s represented a bold step in medical office architecture around …

October 12, 2016
Kaiser’s geodesic dome clinic
There are hospital rounds, and there are round hospitals.
April 20, 2016
Henry J. Kaiser’s environmental stewardship
Since the 1940s, Kaiser Industries and Kaiser Permanente have a long history …
November 13, 2015
Dr. Morris Collen’s last book on medical informatics
The last published work of Morris F. Collen, MD, one of Kaiser Permanente’s …
October 29, 2015
From paper to pixels — the new paradigm of electronic medical records
Transitioning to electronic health records introduced new approaches, skills, …

September 23, 2015
Kaiser Permanente and NASA — taking telemedicine out of this world
Kaiser Permanente International designs, develop, and test a remote health …
July 22, 2015
Kaiser Permanente as a national model for care
Kaiser Permanente proposed a revolutionary national health care model after …

December 11, 2014
Henry J. Kaiser, geodesic dome pioneer

October 8, 2014
Breast cancer isn’t just a woman’s issue

July 23, 2014
Kaiser shipyards pioneered use of wonder drug penicillin
Though supplies for civilians were limited, Dr. Morris Collen’s wartime …
June 24, 2014
Kaiser Permanente's first hospital changes and grows
A collection of vintage photos that chronicle the evolution of Oakland …

September 23, 2013
Kaiser Permanente pioneered solar power in health facilities in 1980
Santa Clara Medical Center hosted a solar panel project in 1979 to demonstrate …